How Vision Correction Procedures Work in Britain
Vision correction procedures have advanced significantly in recent years, offering patients in Britain various options to restore clarity and improve quality of life. From traditional surgical methods to modern lens technologies, understanding how these procedures work can help individuals make informed decisions about their eye health. This article explores the techniques, considerations, and pathways available across the UK healthcare system.
Vision problems caused by clouding of the eye’s natural lens affect millions of people across Britain, particularly those over the age of 60. Modern medical advances have made corrective procedures safer, more effective, and increasingly accessible through both public and private healthcare channels. Understanding the available options, techniques, and what to expect during treatment can significantly ease concerns and help patients prepare for improved vision.
Discovering Alternative Approaches in the UK
Patients in the UK have access to multiple treatment pathways depending on severity, urgency, and personal circumstances. The NHS provides procedures based on clinical need, typically when vision impairment affects daily activities such as reading, driving, or recognizing faces. Private healthcare offers additional flexibility with shorter waiting times and expanded lens options. Some patients explore both routes, attending NHS consultations before deciding on private treatment. Regional variations exist across England, Scotland, Wales, and Northern Ireland regarding referral criteria and waiting periods. Ophthalmologists assess individual cases through comprehensive eye examinations, measuring visual acuity, lens opacity, and overall eye health before recommending specific interventions.
Grasping Contemporary Removal Techniques
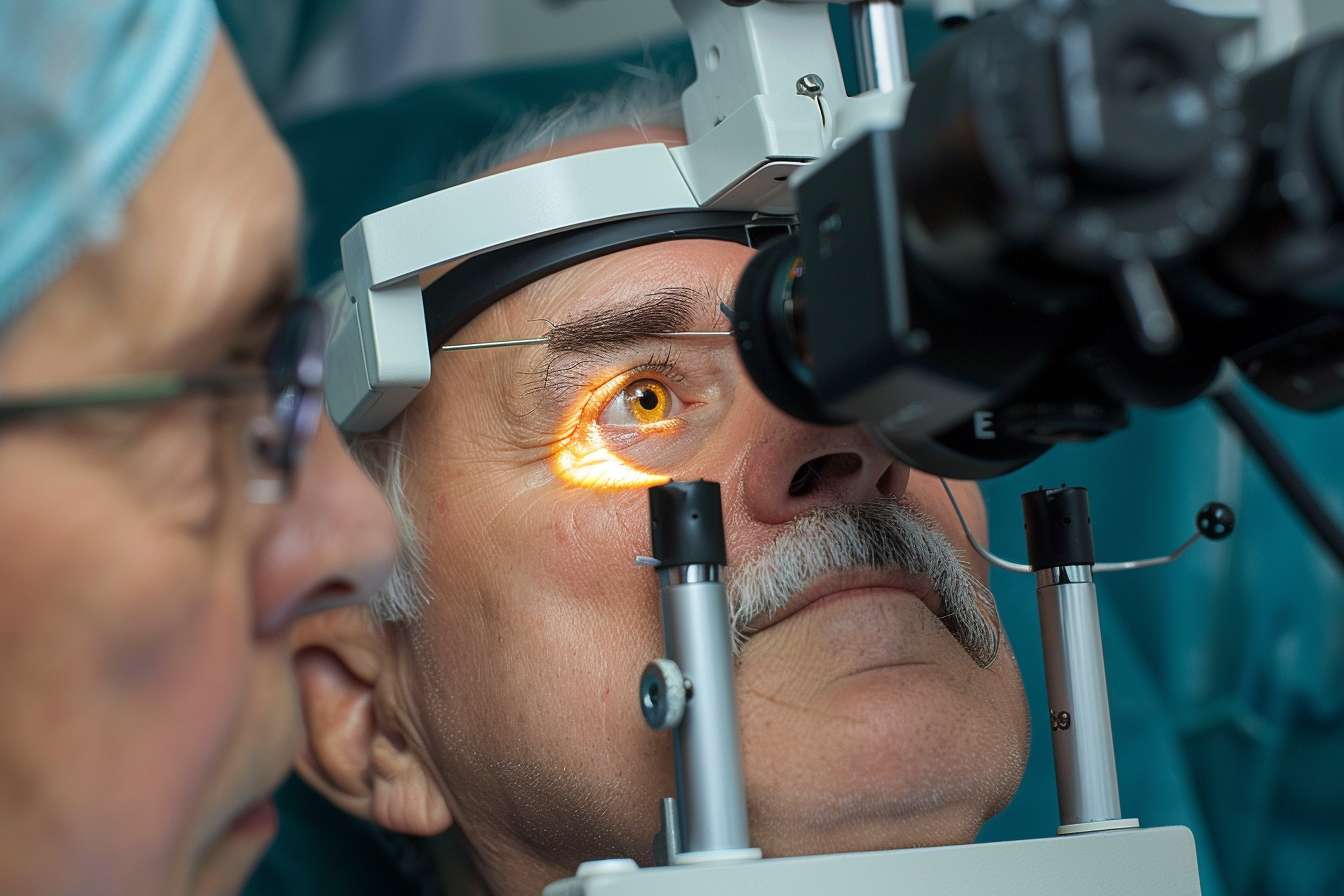
Modern surgical techniques have evolved dramatically from older methods, offering precision and faster recovery. Phacoemulsification remains the most common approach, using ultrasound waves to break up the clouded lens before gentle removal through a small incision. Femtosecond laser-assisted procedures represent newer technology, utilizing computer-guided lasers for enhanced accuracy during critical steps. Extracapsular extraction, though less common today, remains useful for advanced cases with particularly dense lens material. Most procedures take 15 to 30 minutes per eye under local anaesthetic, with patients remaining awake but comfortable throughout. Surgeons create tiny incisions that typically heal without stitches, reducing recovery time and complications. The choice of technique depends on individual anatomy, lens density, and surgeon expertise.
Essential Considerations When Selecting Treatment
Choosing the right treatment pathway involves weighing several important factors. Waiting times differ substantially between NHS and private services, ranging from weeks to several months for non-urgent NHS cases. Lens options vary, with standard monofocal lenses typically provided through the NHS, while private patients may access premium multifocal or toric lenses for astigmatism correction. Cost considerations play a significant role for those considering private treatment, though NHS care remains free at the point of service for eligible patients. Patient lifestyle, visual requirements, and expectations should guide discussions with ophthalmologists. Pre-existing conditions such as diabetes, glaucoma, or macular degeneration may influence timing and approach. Surgeon experience and facility accreditation provide additional quality indicators worth investigating.
The Surgical Process, Recovery, and Lens Choices
The procedure follows a well-established sequence designed for safety and effectiveness. After administering local anaesthetic drops, the surgeon creates a small incision in the cornea, removes the clouded lens material, and inserts an artificial intraocular lens. Most patients experience minimal discomfort during the procedure, reporting only mild pressure sensations. Recovery typically progresses quickly, with many noticing improved vision within days, though complete healing takes several weeks. Post-operative care includes antibiotic and anti-inflammatory eye drops, protective eye shields during sleep, and avoiding strenuous activities initially. Follow-up appointments monitor healing and address any concerns. Lens options include monofocal lenses providing clear distance vision, multifocal lenses reducing dependence on reading glasses, and toric lenses correcting astigmatism. Each lens type offers distinct advantages depending on individual visual goals and lifestyle needs.
Comparing NHS and Private Sector Options in the UK
Understanding the differences between NHS and private pathways helps patients make informed choices suited to their circumstances and priorities. The NHS provides medically necessary procedures based on clinical criteria, ensuring those with significant visual impairment receive treatment. Private healthcare offers faster access, extended consultation times, and broader lens selections. Cost represents the primary distinction, with NHS treatment free for eligible residents while private procedures require payment.
| Service Aspect | NHS Provision | Private Sector |
|---|---|---|
| Waiting Time | 2-6 months typically | 1-4 weeks typically |
| Standard Lens Cost | Free | £2,000-£3,000 per eye |
| Premium Lens Cost | Not routinely available | £3,000-£5,000 per eye |
| Consultation Flexibility | Standard appointments | Extended consultations |
| Lens Options | Monofocal standard | Monofocal, multifocal, toric |
| Surgeon Choice | Assigned | Patient selects |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Understanding Risks and Long-Term Outcomes
While generally safe, all surgical procedures carry some degree of risk that patients should understand before proceeding. Common temporary side effects include mild discomfort, light sensitivity, and blurred vision during initial healing. Serious complications remain rare but can include infection, inflammation, retinal detachment, or secondary clouding requiring additional treatment. Most patients achieve significantly improved vision, with over 95 percent reporting satisfaction with outcomes. Long-term results remain stable, as artificial lenses do not deteriorate or require replacement under normal circumstances. Some individuals develop posterior capsule opacification months or years later, easily treated with a quick laser procedure. Regular eye examinations following treatment help monitor overall eye health and detect any issues early. Realistic expectations, informed by thorough discussions with healthcare professionals, contribute to positive experiences and outcomes.
Vision correction procedures in Britain benefit from advanced medical technology, skilled professionals, and accessible healthcare pathways. Whether through NHS services or private providers, patients can expect effective treatment tailored to individual needs, restoring clarity and enhancing daily life for years to come.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




